Global Health
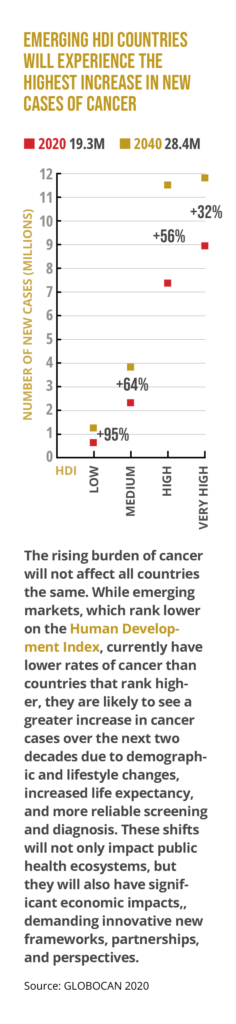
Historically, the World Health Organization (WHO) has led extraordinary efforts to eliminate, and even eradicate, highly communicable diseases such as malaria and smallpox in low- and middle-income countries. The UN-based agency, however, has increasingly turned its focus to noncommunicable diseases, acknowledging the burden that cancer, diabetes, and heart and respiratory diseases are placing on emerging economies.
Cancer emerged as a key topic in 2017 when WHO member states unanimously adopted a landmark resolution, committing to make cancer prevention and control a global public health priority. The following year, the International Cancer Control Partnership—a consortium of cancer control groups from around the world—announced its goal to reduce deaths from noncommunicable diseases, such as cancer, by one-third by 2030.
In February 2020, the WHO released a 180-page report outlining a plan to save 7 million lives from cancer over the next decade by mobilizing stakeholders and strategically using limited resources in low- and middle-income countries.
At the time, however, the attention of national health authorities shifted to the growing threat of the novel coronavirus disease (COVID-19) that had already been reported in Asia, Australia, Europe, and the U.S.
Just four weeks after the report was released, the WHO declared the COVID-19 outbreak a global pandemic.
COVID-19-Related Disruptions Will Result in Additional Cancer Deaths
The COVID-19 pandemic has resulted in major setbacks for cancer-fighting efforts around the globe. Not only are cancer patients at higher risk from COVID-19, but 42% of countries reported disruptions in cancer treatment due to the pandemic’s strain on their healthcare systems, according to the International Journal of Cancer.
Cancer screening programs were particularly affected. One study showed breast cancer screening rates in Taiwan down by more than 20%. In the Netherlands, colonoscopies fell by 45%. Lung cancer scans in the U.S. dropped by more than 70%.
The widespread impact will become more evident in 2022. UK researchers project significant increases in premature cancer deaths due to missed screenings over the next five years, estimating as many as 150,000 more deaths from colorectal cancer, 95,000 from lung cancer, 65,000 from breast cancer. and 32,000 from esophageal cancer in the UK alone.
New Approaches to Awareness and Detection Will Emerge
With global health officials optimistic that COVID-19 could begin to recede as a public health emergency in 2022, countries are urged to develop COVID-19 recovery plans that address disruptions to health services in the short term, while also promoting long-term policies to build more resilient healthcare systems in preparation for future pandemics.
Awareness and early detection will continue to play a key role. Increased availability of telehealth services—access to which has expanded during the pandemic—is a much-needed health policy intervention to bolster awareness campaigns. They can be aided by increased deployment of at-home screening tests that have been developed for several cancers as well as community- based programs for cancer screenings that cannot be performed at home. The use of wearable devices to monitor patients undergoing cancer therapy should become more common.
However, with government resources and healthcare workforces depleted by COVID-19, government health ministries alone cannot launch a holistic post-pandemic response. A multistakeholder approach that ensures the best use of limited resources, pools expertise, and considers different perspectives will be needed.
The WHO’s February 2020 cancer report specifically called on countries to adopt more effective National Cancer Control Plans (NCCPs) by including private sector and nonprofit organizations in their design and implementation.
A robust NCCP should tackle the range of cancer-related interventions: primary prevention, screening and early diagnosis, access to treatment and services, and evaluation, governance, and monitoring of implementation. It also requires convening representatives from industry, academia, and patient advocacy and provider groups, along with health ministry officials, to identify the highest priorities and the most cost-effective responses.
Cervical Cancer Will Pave the Way for Other Specific Campaigns
While efforts to fight all kinds of cancer will get renewed attention, efforts to eliminate cervical cancer will be heightened in 2022.
In 2018, the WHO called for the elimination of cervical cancer by 2030 through a combination of increased access to screenings and treatment as well as widespread uptake of vaccination against the human papillomavirus (HPV), which causes the vast majority of cervical cancers.
Though vaccination and screening campaigns were hindered by the pandemic, numerous organizations are poised to redouble their efforts in the coming year. For example, in August 2021 the Asia-Pacific Economic Cooperation (APEC) forum, with 21 member economies, issued a road map for forming multisectoral partnerships to defeat cervical cancer. The strategic objectives aim to support APEC economies in accelerating and scaling prevention of cervical cancer through HPV vaccination of eligible populations and effective screening and treatment of pre-cancerous lesions, expanding the application of health-systems tools to improve the quality of treatment and palliative care and improving health infrastructure to support improvements in prevention and care.
Look for the most successful strategies in this effort to be employed in other cancer-fighting campaigns in the future.